Is it Plantar Fasciitis?
Many times, pain in the bottom of the foot or heel can be pushed into a blanket diagnosis of “you have plantar fasciitis”. But is it plantar fasciitis? Could it be another condition like tibialis posterior tendonitis, stress fracture in the heel, radiating pain from the low back? While getting a blanket diagnosis of plantar fasciitis based on zero exam with some basic rehab and soft tissue techniques thrown at it may work, there is a good chance it probably will not. You must know what you are aiming at. And in the same boat, what is causing the plantar fasciitis? Just because there is pain and inflammation in the plantar fascia does not mean that the CAUSE of the pain is coming from that area as well. In fact, it rarely does. This is why seeking out help from sports chiropractor or physical therapist is important to get a proper diagnosis and most importantly find out the main cause of the pain.
For the purposes of this blog, we will assume that we have ruled out all red flags, low back, and other conditions near the foot. We will focus on differentiating between plantar fasciitis and tibialis posterior tendonitis. We will go through anatomy and function, classic signs of each condition, and patient history things to consider. In the next blog we will go through treatment and rehab considerations for each condition.
What is the Plantar Fascia?
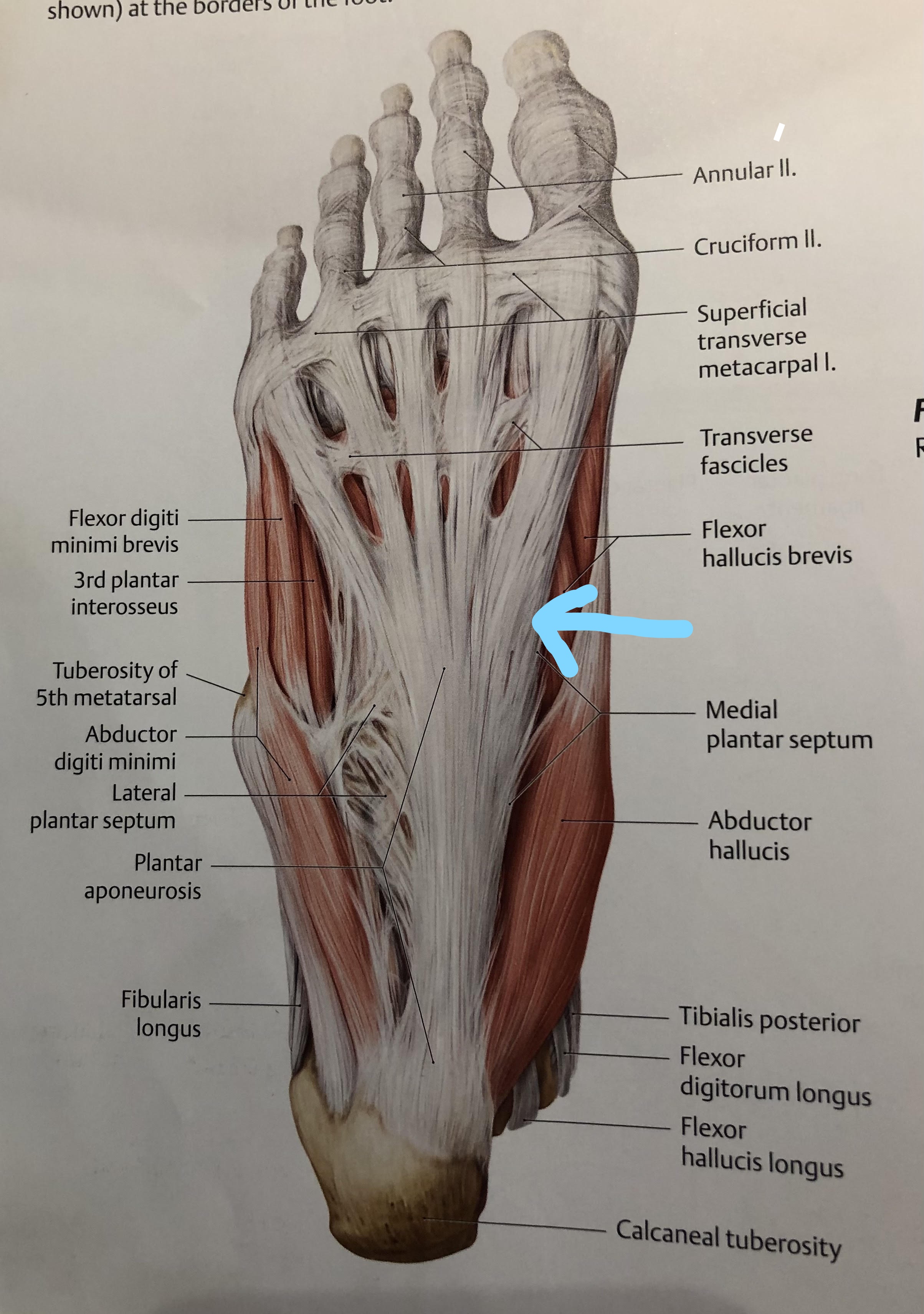
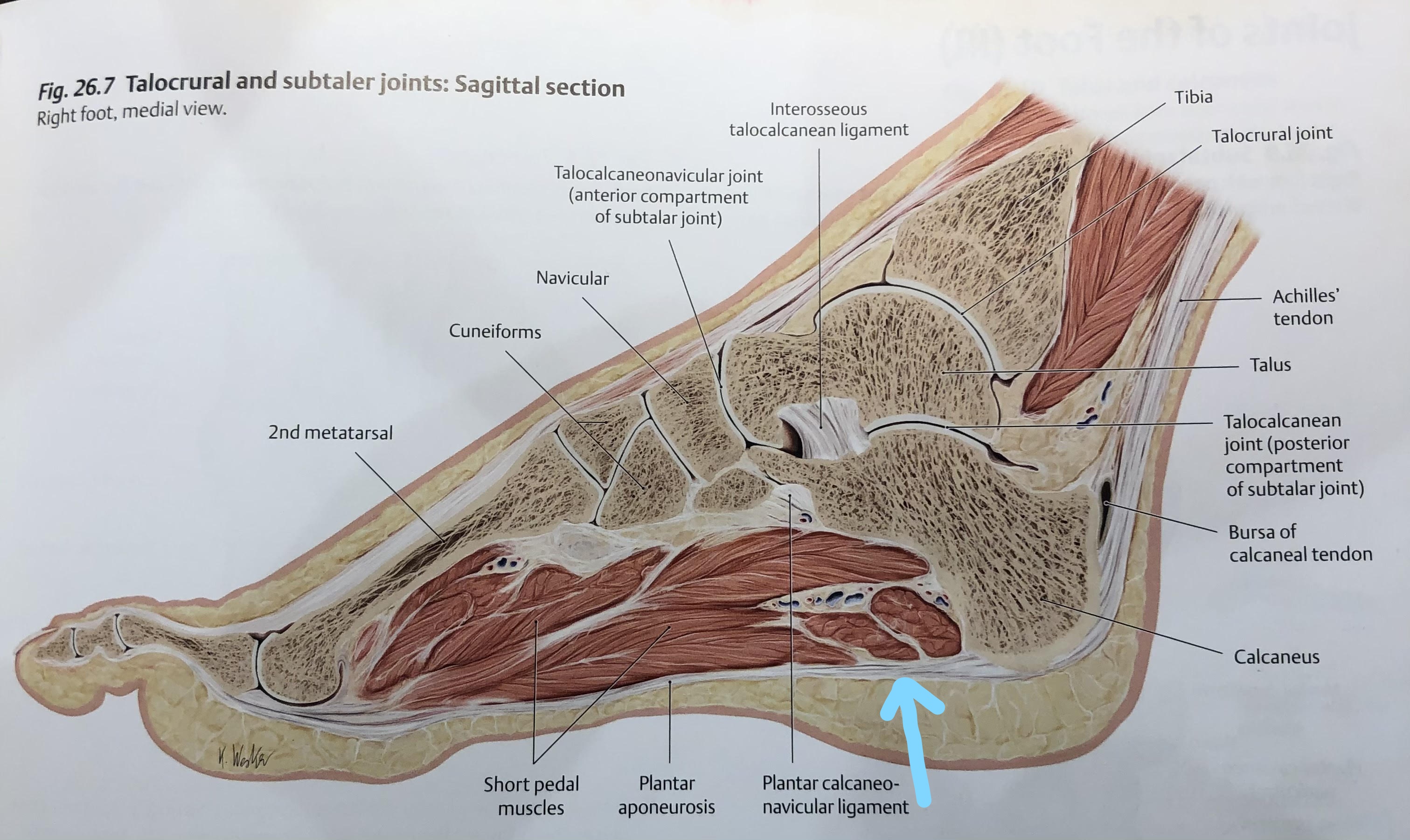
The plantar fascia is a dense, fibrous connective tissue that is attached to the heal, toes, and many surrounding muscles and structures of the bottom of the foot. The plantar fascia is designed to be a passive (meaning non contracting) transmitter of forces that are put on the foot. It is also a supporter of the medial longitudinal and transverse arches.
What is the Tibialis Posterior?
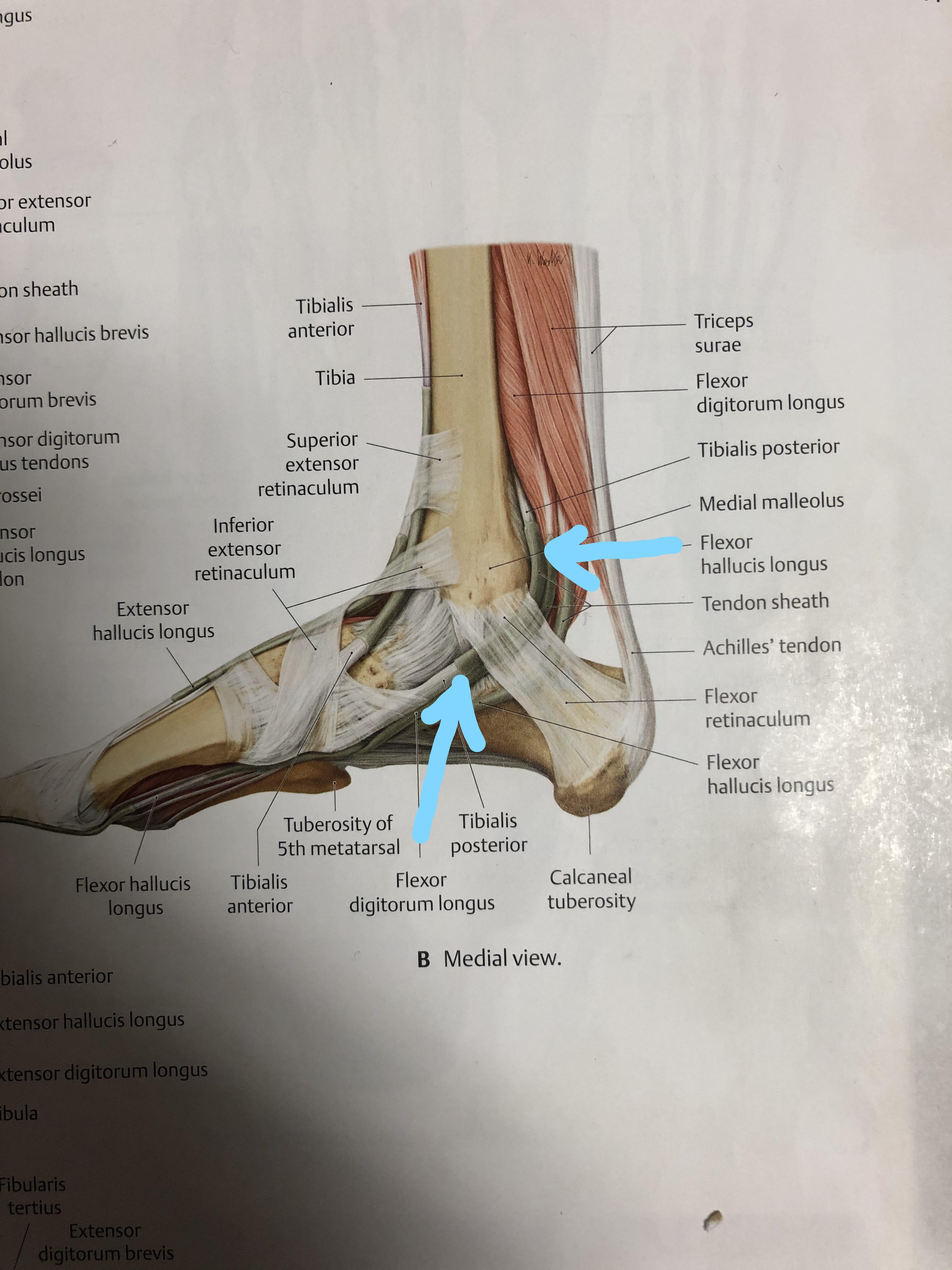
The tibialis posterior is the deepest and most central muscle of the lower leg with fibers originating on both shin bones. It wraps around and inserts into the calcaneus, navicular, cuboid, cuneiforms, and the second through fourth toes. With it location, multiple attachment points, and powerful tendon, it is the most important stabilizer of the foot helping to create the medial arch. When injured or weakened, stabilization of the foot can be compromised. The tibialis posterior also helps to flex the ankle down and turn in.
Plantar Fasciitis Classic Signs:
- Pain with first steps in the morning or prolonged period of rest.
- Pain again comes back usually toward the end of the day with increased weight bearing activity.
- Walking on toes or upstairs can be aggravating
- Diffuse pain across heal or pinpoint pain on bottom of heal
- Tenderness along inner side of bottom toward heel
Tibialis Posterior Tendonitis Classic Signs:
- More pain in heel longer you are on it
- Pain along medial border of foot to behind medial ankle and up medial posterior shin
- Pinpoint pain and tenderness at the navicular (bone behind the tissue of the bottom arrow in tibialis posterior picture above).
Recent History:
- Any sudden increase in activity like running or explosive movements over last few weeks or months.
- The increased strain from activity alone could have been too much for the body to adapt and recover from.
- Any change in footwear whether for work or workouts.
- Improper footwear can put the toes in relative upward position for longer periods of time causing the fascia to be consistently overstretched over time.
- Improper footwear can also cause the foot to become stiff from lack of movement. Very stiff and rigid shoes that allow minimal movement in the foot cause this to happen over time. Then when the demand is placed on the foot and it needs to be mobile, it cannot move properly and leads to pain. This is why we refer to some shoes as a “coffin for the feet”. They do not allow the foot to be a strong and mobile base of support leading to the “death” of its very important function.
Flat Feet and Pronation
A big misconception we hear is that a patient’s pain is due pronation or their “flat fleet”. The reality is people with high arches can get plantar fasciitis and people with “flat feet” are not doomed to come down with it. It is more about the rate at which you can control pronation and how long you remain in it that it the problem. People who overpronate or cannot control the rate of it, will elongate the fascia like wringing out a dish rag that will cause increased strain on the fascia. This foot is too mobile.
People that cannot move properly through the foot limit their shock absorption and cannot dissipate forces, so the fascia takes a beating. This foot is too rigid.
Stayed tuned as we will cover how treatment for people that cannot control pronation vs people that cannot move properly throught the foot can be different, as well as general treatment and rehab considerations for each condition in the next blog!
References: Gilroy, A. M., MacPherson, B. R., & Ross, L. M. (2008). Atlas of anatomy. Stuttgart: Thieme.
About the author
When it comes to mechanical pain, Dr. Tyler Panko has seen the best outcomes produced when chiropractic, physical therapy, strength and conditioning, and soft tissue techniques and principles are combined into an individualized plan for the patient. His purpose and passion are to educate and help all people, ranging from acute to chronic pain, professional athlete to daily worker, and young child to elderly, go from pain to increased performance in their daily lives doing the things they love. His belief is that life is an athletic event, and everybody has the right to move and feel great well into old age.
